Your trusted source for contextualizing the news. Sign up for our daily newsletter.
As COVID-19 began to sweep the country three years ago, members of Congress banded together to pass the overwhelmingly bipartisan Families First Coronavirus Response Act to address the public health crisis.
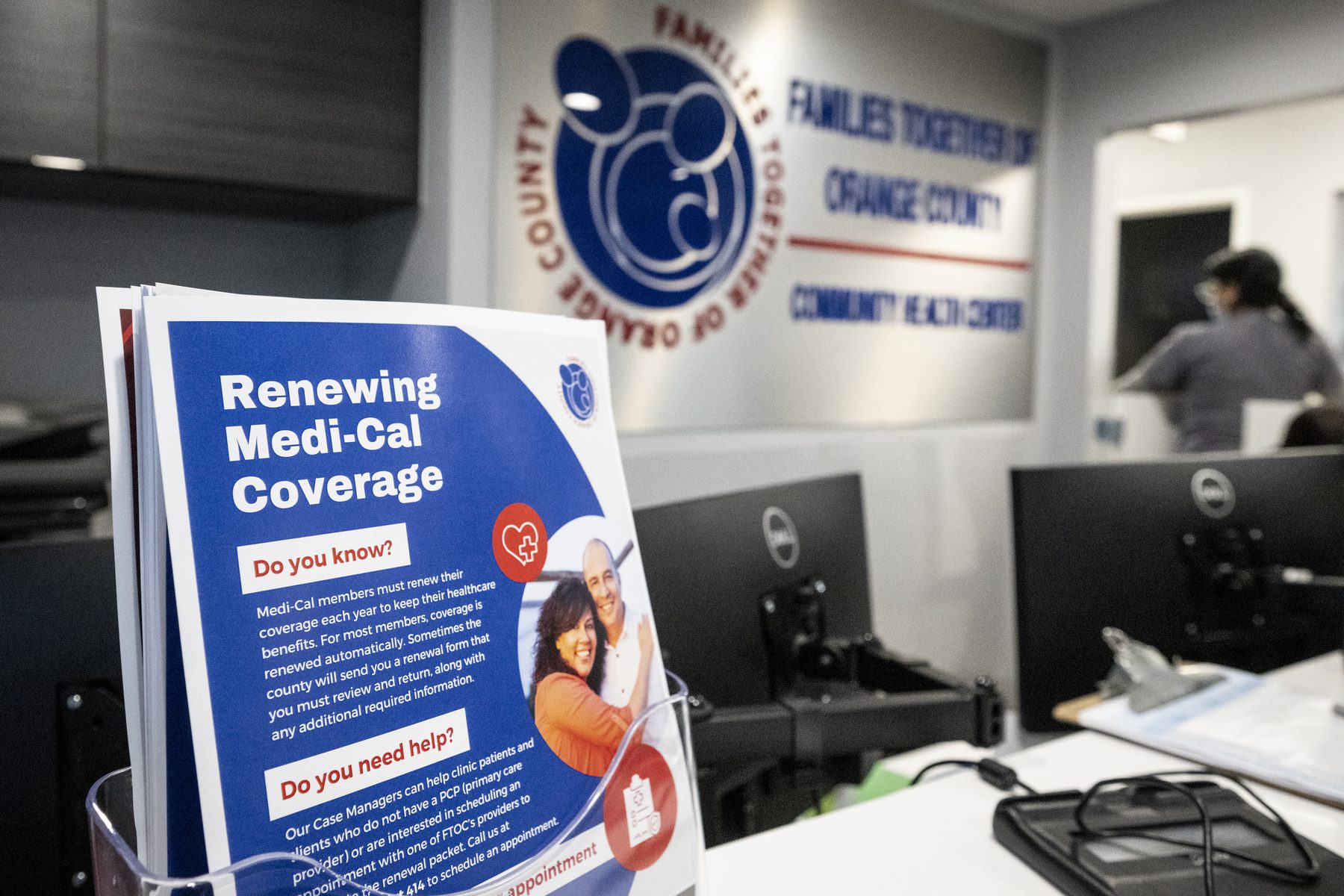
The legislation funded free coronavirus testing, 14-day paid leave for many workers impacted by the pandemic and increased funding for food stamps. It also mandated that Medicaid, the health care program for low-income people, keep beneficiaries continuously enrolled through the COVID-19 public health emergency. This meant that although new beneficiaries could enroll in Medicaid during the pandemic, no one who was eligible for coverage as of March 18, 2020, could lose coverage.
Since the Families First Coronavirus Response Act was enacted in 2020, Medicaid enrollment has grown by over 30 percent. Between February 2020 and November 2022, 20.5 million new people were enrolled in Medicaid coverage.
Among those most impacted by the continuous enrollment provision are pregnant and postpartum people. Federal law mandates that states provide pregnancy-related coverage through 60 days postpartum, but in America’s pregnancy-related death crisis, many deaths occur after that period. Since March 2020, postpartum coverage has been continuous, helping people to access potentially lifesaving care.
The continuous enrollment is set to end at the end of this month, and millions of people are soon expected to lose coverage. These include the postpartum people who were able to access care, people who have gotten new jobs during the pandemic but are still below the poverty line and young adults who have aged out of coverage they had as children.
Although some people who lose Medicaid coverage will be able to access coverage through the federal insurance marketplace, many will not. That is in part because the income eligibility threshold in states that have chosen not to extend Medicaid programs remains incredibly low, leaving many to fall in the coverage gap.
The 19th spoke with Allexa Gardner, a research associate at Georgetown University’s McCourt School of Public Policy, and Jennifer Tolbert, the director of state health reform and associate director for the program on Medicaid and the uninsured at the Kaiser Family Foundation, to understand the disenrollment process, what it means and what to do if coverage disappears.
The Medicaid disenrollment process may look different depending on the state. What will be uniformly happening across every state?
Across the board, every state is going to conduct a full redetermination of eligibility for every Medicaid beneficiary. That means a review of about 84 million people who are currently enrolled in Medicaid.
Eight states began this redetermination process in February, while 15 began in March and 28 will begin the process in April. All states are required to start the renewal process by setting an ex parte renewal, meaning they are looking through available data systems, like wage databases, to try and determine someone’s eligibility without having that person provide proof of eligibility.
“The ability to do those automatic renewals where a beneficiary doesn’t have to do anything can range from less than 25 percent of renewals being completed that way to over 75 percent depending on the state,” Gardner said.
-
More health coverage
- From formula to medications and child care, parents are being crushed under a wave of shortages
- As states seek to scale back abortions, Montana wants to redefine medical necessity under Medicaid
- For young people on Medicare, a hysterectomy sometimes is more affordable than birth control
The Centers for Medicare and Medicaid Services (CMS) has given states 12 months to initiate the renewals and 14 months to fully complete the renewal process. But Tolbert noted that while 43 states are planning to take 12 to 14 months to complete all renewals, some states are moving more quickly.
“The challenge there is that the more quickly a state moves, the more renewals it will be processing in each month. Therefore, there is a greater burden on staff and more opportunities for issues to arise with processing the renewals.”
When will people begin losing Medicaid coverage?
As early as April 1. Of the states that initiated their eligibility verification process in February, five anticipate that they will begin termination in April: Arizona, Arkansas, Idaho, New Hampshire and South Dakota.
How will people be notified of their enrollment status?
Via mail. Tolbert also noted that every state has allowed enrollees to create online accounts where they can receive updated information.
How many people are expected to lose coverage during the disenrollment process?
KFF estimates that between 5 million and 14 million people will lose Medicaid coverage. This estimate is a bit lower than the 15 million people that the Department of Health and Human Services (HHS) estimates will lose coverage.
Who is most at risk of losing coverage?
Children will be among the people most at risk of losing coverage. It is estimated that 70 percent of children who are currently enrolled will lose coverage even though they will remain eligible for Medicaid. Confusion is expected to arise from the fact that states’ eligibility level for children varies greatly from the eligibility level for adults.
“Even if a parent loses eligibility, their child may still be eligible, but parents may not understand or be aware of that,” Gardner said.
Gardner noted that most children who are no longer eligible for Medicaid should remain eligible for coverage through the Children’s Health Insurance Program (CHIP), which provides coverage to children in families with incomes too high to qualify for Medicaid, but not high enough to be able to afford marketplace coverage.
Postpartum people will also be greatly impacted. As a provision of the American Rescue Plan, the robust economic stimulus legislation that was enacted in March 2021 to provide economic relief amid the pandemic and recession, states have the option to extend Medicaid postpartum coverage to 12 months instead of 60 days. Thirty states have chosen to implement this 12-month extension.
Amid the ongoing, pregnancy-related death crisis, there are eight states that do not have legislation that has been enacted or is pending to extend Medicaid coverage for postpartum people. In three states, including Texas — the state with the highest number of uninsured residents and highest percentage of women of childearing age — a limited coverage provision has been proposed, but not passed.
What does it mean to be disenrolled for procedural reasons?
HHS estimates that 6.8 million people will lose coverage even though they are eligible for the program. These procedural disenrollments may occur when a person doesn’t receive their renewal notice, can’t provide documentation required by the state, or doesn’t submit their documents by the deadline indicated on the renewal request form.
Although all states must give enrollees based on modified adjusted gross income (MAGI) 30 days to respond to a renewal request, states are not required to do more than send out the renewal form and a 10-day termination notice if the enrollee does not respond.
According to KFF, Medicaid enrollees are more likely to be transient or face barriers because English is not their first language. But Gardner notes that these procedural disenrollments are not inevitable.
“How many people lose coverage inappropriately or for those procedural reasons is really going to depend on how well a state does with this process,” she said.
What should people do if they are disenrolled for procedural reasons?
People disenrolled for procedural reasons should submit the missing information or renewal notice to their state Medicaid agency. They can also contact the Medicaid agency to try to have coverage reinstated. States must provide a 90-day reconsideration window in which people in MAGI groups can provide the needed information to reestablish eligibility without having to complete a new application.
How do people appeal a disenrollment if they submitted everything and are deemed ineligible?
People can file an appeal and a fair hearing request, a process in which they can challenge a denial to the state Medicaid agency. There is a process in which the state has to reexamine the case and take a look at any new information that may be available to reassess eligibility.
Where can people go for assistance filling out verification forms?
In every state there are people to assist with applications, called navigators. They are required under the Affordable Care Act and typically help people sign up for marketplace coverage, but they also help people apply for and renew Medicaid coverage. Individuals can access navigators here.
What happens if people are deemed no longer eligible for Medicaid?
Undoubtedly, many people will fall in the coverage gap, especially if they live in states that have not expanded Medicaid. Still, there is hope for some people who are no longer eligible for Medicaid to access coverage in the marketplace. Health care navigators can help people better understand their options during this transition.