Your trusted source for contextualizing health news. Sign up for our daily newsletter.
A federal judge in Texas struck down the legal requirement that health insurance plans cover the HIV prevention pill at no cost, as well as a range of other preventive services, including many that improve reproductive health.
The national injunction, issued Thursday, threatens to undo one of the Affordable Care Act’s most significant gender-based health reforms. The decision is not a surprise — Judge Reed O’Connor signaled he would rule this way in a decision last September — but it was not clear until now just how broad an injunction he would grant. The Affordable Care Act (ACA), now more than 13 years old, has emerged as a centerpiece of President Joe Biden’s health agenda, and he has touted his administration’s efforts to expand on the law’s insurance protections.
“The decision is really really significant,” said Andrew Twinamatsiko, associate director of the O’Neill Institute at Georgetown Law School. “The most vulnerable of our populations are going to be most affected.”
The ruling is likely to be appealed to the U.S. Court of Appeals for the 5th Circuit, which is considered one of the most conservative appeals courts in the country. After that, it would go to the U.S. Supreme Court.
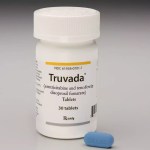
The case at hand involves a legal challenge to the ACA provision requiring health insurance to cover certain preventive services with no out-of-pocket cost to patients. Those benefits are picked by the U.S. Preventive Services Task Force, the Health Resources and Services Administration, and the Advisory Council on Immunization Practices. They include the daily pill taken for HIV prevention — known as pre-exposure prophylaxis (PrEP), which is 99 percent effective — as well as at least one version of each method of contraception.
-
Previous Coverage:
-
Previous Coverage: The Affordable Care Act’s biggest gender-based protections are under threat
The plaintiffs, a group of employers, argued that the U.S. Constitution does not allow the government to let those bodies determine which services are covered. They also claimed they should not have to provide insurance covering PrEP and contraception, saying doing so violated their religion, arguing that covering those benefits would make them “complicit in facilitating homosexual behavior, drug use, and sexual activity outside of marriage between one man and one woman.”
The ruling eliminates health insurance plans’ requirement to cover without cost-sharing any benefits articulated by the Preventive Services Task Force. Those include HIV screening, chlamydia and gonorrhea screenings, breastfeeding support, mental health interventions for pregnant and postpartum people, and counseling and treatment for people at higher risk of breast cancer. Medication for breast cancer chemoprevention, meant to help reduce breast cancer risk, could also be subject to cost-sharing following the judge’s decision.
Screenings recommended by the task force prior to the signing of ACA on March 23, 2010, would still be covered without out-of-pocket costs for patients. This is expected to include mammograms, colorectal cancer screenings and cervical cancer screenings, said Alina Salganicoff, senior vice president and director of women’s health policy with the Henry J. Kaiser Family Foundation (KFF).
Patients’ out-of-pocket costs for the screenings affected by the ruling will vary wildly depending on the type of insurance plan, deductible and cost-sharing requirements of a particular plan. Research indicates that even small amounts of cost-sharing reduces the likelihood that people will use those services, Salganicoff said.
O’Connor, who has previously ruled in favor of challenges to the ACA, also held that insurance plans cannot be required to cover PrEP, citing the plaintiffs’ religious objections. That particular decision could have significant implications for the grounds under which people use religion-based arguments moving forward.
“This is really expanding what claims can be made under the Religious Freedom Restoration Act,” Twinamatsiko said. “We see a claim rooted in homophobia gaining the day in court and the court endorsing it.”
-
More from The 19th
- Health care for transgender adults remains legal, but states are quietly trying to limit access
- The 19th Explains: Who will be most impacted by Medicaid changes — and when
- Only 1 percent of abortions in Utah took place in a hospital. Soon, that’s the only place they’ll be allowed.
O’Connor dismissed the arguments against the ACA’s birth control benefits, which are not determined by the Preventive Services Task Force, arguing that the plaintiffs had not shown they had legal standing to challenge that provision of the law. That means that for now, people should be able to continue getting contraception with no out-of-pocket costs.
Both sides of the case will likely appeal the decision, Laurie Sobel, associate director for women’s health policy with KFF, told reporters Thursday. The Biden administration will appeal the argument in O’Connor’s ruling, and the plaintiffs in this case will likely seek an expanded ruling in favor of striking recommendations by the Advisory Committee on Immunization Practices (ACIP) as well as the health law’s contraceptive mandate, which falls under the Health Resources and Services Administration (HRSA). ACIP and HRSA recommendations are among the most commonly used services for individuals, including “Well Women” and “Well Child” care visits, KFF told reporters.
“Nobody’s happy with this decision,” Sobel said. “So all of the preventive services are kind of up for grabs as we go through the appeal process to the 5th Circuit and to the Supreme Court.”
“We’re not out of the woods yet,” Twinamatsiko said.
For small group and individual health insurance plans, benefits are set before the year starts and cannot change for the calendar year, which means that people covered through those options would not see any changes until 2024.
But for those who get health insurance offered by large employers — the biggest single source of health care in the United States — the impact could be seen sooner, as many plans now have the option to drop or scale back their preventive benefits at any time, introducing co-pays or other forms of cost-sharing. That said, if the case is likely to be appealed, health insurers may decide it is too logistically unpredictable to keep changing their benefits without knowing what the final decision is likely to be.
About 100 million people use ACA-protected preventive services in a given year, according to KFF. Since the preventive services mandate took effect, Twinamatsiko said, research has shown that Black and Latinx Americans faced fewer barriers to getting preventive health services.
Blocking the mandate, he added, means “we’ll again be going back to see a widening of gaps.”