In the hours after Roe v. Wade was overturned, frantic emails began spilling into Dr. Robert Hunter’s inbox. But his patients weren’t asking about abortion, the procedure Roe had protected since 1973. They were asking about their embryos — specifically, whether they should move them.
Hi Dr. Hunter, I just wanted to check in and see if there is anything we need to be worried about…especially with 6 frozen embryos.
Hi Dr. Hunter! … Since the overturn of RvW, I’m now a little nervous about our future and not sure if I will have all of these choices later on down the road.
Dr. Hunter, Has your clinic discussed measures to potentially move/protect the stored embryos now that Roe has been overturned this morning? I may be ignorant, but I had a moment of worry our embryos might be at risk to folks who don’t understand.
Hunter runs a fertility clinic offering in vitro fertilization (IVF) in Louisville, Kentucky, where a blocked abortion law could soon put IVF in jeopardy, too. Now, many patients are scrambling to make decisions about their future. Kentucky is one of a handful of states that wants to use an abortion regulation to define life as beginning at fertilization, common language that is present in several other abortion bans that have gone into effect or will soon, including in Utah, Texas and Louisiana.
The Kentucky law is currently blocked by courts, but that could change soon and, in November, voters will determine whether the state can even guarantee the right to an abortion.
Other states want to move further, giving embryos constitutional rights through what are called “personhood” bills, even though, scientifically, most will never become babies. Roe was the largest roadblock stopping these kinds of bills from becoming reality, but without it, patients in states including Iowa, Ohio, Oklahoma and South Carolina, where personhood laws have been proposed but have not yet passed, could face the same questions as Hunter’s patients in Kentucky.
Both kinds of laws could affect embryos created through IVF, causing spillover effects into other areas of reproductive care. Hunter’s patients likely now have a small window before those laws become more concrete realities in Kentucky, putting into question what they can do with their own embryos. Moving embryos to another state could buy patients some time. It may also afford them something even more valuable: a choice.
“IVF is just another side of the reproductive choice coin,” Hunter said. “You think about abortion as being a woman’s right to choose ‘no.’ IVF is their right to choose ‘yes.’”
After Roe was overturned, Kenyon Laing was one of the patients trying to reach Hunter’s clinic, where her two remaining embryos are stored.
After the decision came down June 24, she marched with her husband at a protest in downtown Louisville, visibly pregnant at 23 weeks with a baby conceived through IVF. “Pregnant and pro-choice,” she chanted in the 92-degree heat. But it was the first time she’d stood at a protest feeling that no matter how much she shouted, her voice wouldn’t carry — Roe was gone, and at least in Kentucky, there would be little to stop what could come next.
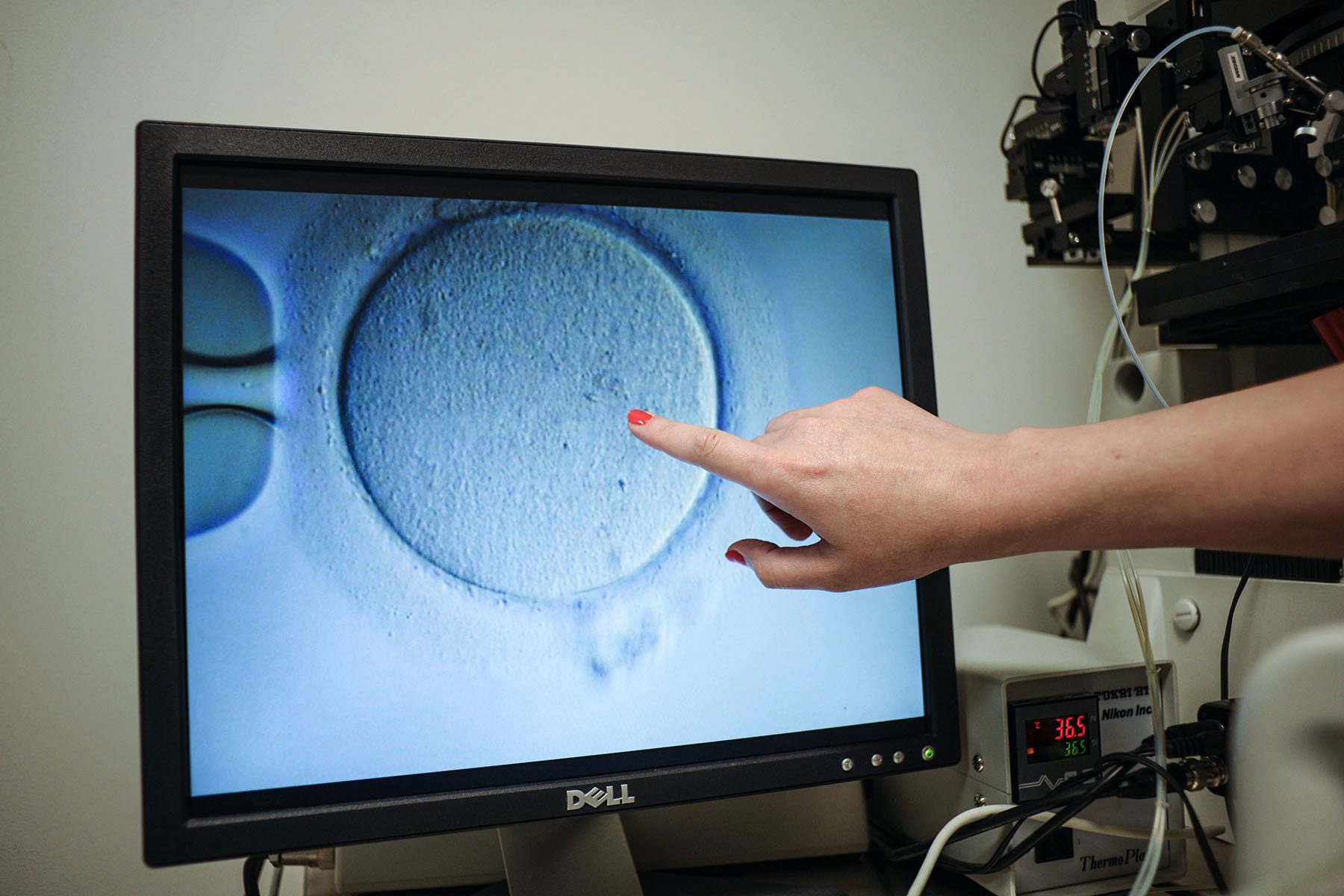
Laws that define life as beginning at conception could lead to limitations around how many eggs are fertilized in each IVF cycle and whether the resulting embryos, most of which are often not genetically viable, can be disposed of. It’s standard to retrieve a dozen eggs or more, then fertilize and test them to ensure the one that is implanted in the uterus has the best chance of leading to a healthy pregnancy. In Laing’s IVF cycle, for instance, Hunter retrieved 40 eggs and fertilized about half. Of those, 13 actually fertilized successfully and only three were ultimately high quality enough to likely lead to a live birth.
-
The Latest:
If those embryos are considered people from the moment they’re fertilized, disposal could be a crime and doctors could be prosecuted. That would make IVF less successful, more costly and more inaccessible.
The week after Roe was reversed, Laing typed an email to Hunter: Given the Supreme Court’s recent decision, my husband and I would like to move our embryos to storage in a different state (Minnesota) as soon as possible.
Hunter wrote her back right away. Most reproductive endocrinologists currently recommend not moving embryos until they know exactly how abortion regulations may impact IVF, he told her. It’s still unclear how direct an effect they could have because so much of the language is vague and doesn’t directly address the procedure. Kentucky’s bill, for example, defines an unborn child’s life as beginning from the moment of fertilization, but other bills, like Ohio’s, go further to specifically confer constitutional rights on “all unborn human individuals from the moment of conception.” Moving embryos before it’s clear how those definitions could limit IVF would introduce some risk, however small, that something could happen to the embryos in transit, doctors argue.
Typically, embryos are stored in liquid nitrogen inside cryopreservation tanks either onsite at clinics or in larger storage facilities. Clinics work with private companies to help shuttle embryos from state to state, which is often done if a patient moves.

It’s the same system patients like Laing are tapping into now, worried that the legal landscape in their states could shift.
“I just don’t feel comfortable living in a state where a doctor has to make a decision about whether or not they could go to prison to save my life,” she said.
Laing is now in the process of setting up care with a new doctor in Minnesota, where her parents live and where the right to abortion is protected under the state constitution. Hunter helped connect her with Cryoport, a leader in cryopreservation and embryo transport, that will move her embryos from Kentucky to the new clinic. It’ll cost at least $780, plus annual storage of about $750.
The decision feels in some sense like a reclaiming of the autonomy she’s lost in her journey to parenthood.
Laing’s first miscarriage was on her birthday in August 2020, followed by a second loss in November of that year. She turned to IVF because it offered her more surety than her body could. Her first child is due in October.
But IVF — the injections and medications and procedures — took a toll on her body, and the first 18 weeks of her pregnancy passed in a haze of nausea. Her experience trying to conceive a child only strengthened her resolve that people should choose this journey.
“To be forced to carry, to be forced to remain pregnant — it’s barbaric,” said Laing, 34. “I consider myself beyond pro-choice now. I am pro-abortion, and that is really informed by the experience of my body going through all of this.”
A deluge of requests are now hitting fertility doctors in most states — those with potential personhood bills and those without, where the embryos could be moved.
In Seattle, Dr. Lora Shahine, a reproductive endocrinologist at Pacific NW Fertility and host of the Baby or Bust Podcast, said every single patient she’s had since Roe was overturned has asked her about how the decision could affect their treatment. Calls are coming in from out-of-state patients who want to establish care with Shahine so they can then move their embryos to Washington, where the right to abortion has been codified for more than 30 years.
Those she’s spoken to are worried their embryos could be held hostage by abortion legislation and that they’d then be unable to move them out of state, Shahine said. They are worried their state will force them to have another child even though they feel their family is complete. They are worried about getting pregnant at all and miscarrying — will they be able to receive the care they need?
It’s not a question for Shahine whether she wants to help them but whether, logistically, she can.
Cryopreservation takes space. Pacific NW Fertility stores its embryos onsite, but it’s expensive, and purchasing more square footage is costly in Seattle. The clinic offers some offsite options for long-term storage out of state through partnerships with cryopreservation companies, but those options are expensive and already limited.
“We have to get together as a clinic and think, ‘How many of these patients can we accommodate?’” Shahine said. “The more outside of the state we are accommodating, the less people here in Seattle who want our care are going to be able to get our care. How do we balance that?”
Dr. Stephanie Gustin, the medical director at the Heartland Center for Reproductive Medicine in Omaha, one of the only two fertility clinics in Nebraska, is also fielding questions daily. Gov. Pete Ricketts is weighing whether to call a special session to reintroduce an abortion ban with a conception standard this summer. When the bill was first introduced earlier this year, it failed to pass by only two votes. Ricketts said a new version will likely have to be introduced and it wouldn’t affect IVF, but reproductive endocrinologists in the state, including Gustin, are campaigning to block the legislation altogether.
In the meantime, she’s also in touch with cryopreservation companies, who have told her they intend to facilitate the transport of embryos for doctors and clinics if laws were passed that limited doctors’ ability to handle embryos.
“Those companies have told us that if a patient wants to discard an embryo because it’s genetically not normal or nonviable, but [they’re] in the state where they may not be able to do that otherwise, they would be able to do that on their behalf,” she said. Cryoport and ReproTech, two of the leaders in that space, did not reply to multiple requests for comment.
Other companies are also stepping up to offer more transport services. Just hours after Roe was overturned, Lilia, a Toronto-based start-up that specializes in freezing eggs, launched a new service to move embryos across states to a partner facility in Massachusetts, a state that has codified the right to an abortion.
Lilia offers to do all the legwork for patients, contacting their provider and clinic and setting up transport and storage. Transport is about $970 and annual storage is $495, but the company hopes to bring those costs down as it fleshes out the model, said CEO Alyssa Atkins.
“Our approach is to be here and be of service. We are not looking to make huge profits off of this service,” said Atkins, who has already started to hear from patients who are interested in moving embryos. “The risk for folks who are creating embryos is that these ‘personhood’ bills could make an already expensive process five to six times more expensive.”
In the legal gray area created since the fall of Roe, patients who have embryos in storage are stuck with few clear answers as to how — and when — they should make a decision.
In Georgia, Sydney Bauer and Liz Reynolds just finished their ninth intrauterine insemination (IUI) cycle. If this latest IUI attempt doesn’t work, they are planning on starting IVF.
As a queer couple, they have begun working with their fertility clinic to make sure the sperm they have banked up can be put under Reynolds’ name. Bauer, a transgender woman, is worried her sperm she banked before beginning to medically transition may be unusable, but not for any medical reason. The couple fears that any forthcoming attacks on LGBTQ+ rights could endanger their own biological materials.
“People don’t realize, and I didn’t realize until I started to medically transition, just how interconnected reproductive health care is with so many other aspects of health care,” Bauer said. “The ways people are working to restrict abortion will have so many trickle down effects for not just cisgender women, but for trans people across the country … This is about everyone.”
Living in Georgia, where personhood rights routinely come up in bills introduced in the state legislature, the couple has had to consider whether they should leave their home of 12 years for the sake of a future family. “We’ve had conversations — ‘OK, if we do move forward with IVF, do we move forward with this clinic or do we move and do this in New York or do we stay here and travel back and forth?’” Reynolds said.
Adding to the pressure is the reality that a grant they received from the Jewish Fertility Foundation to help cover the costs of their fertility treatments expires in September. One cycle of IVF costs patients about $23,000 on average, so if they need to undergo the procedure, they must do so as soon as possible.
In Atlanta, Monica Caron also isn’t sure can wait much longer. She has one frozen embryo left after welcoming a daughter through IVF in the fall of 2020. She had been hoping to wait at least another year before beginning an IVF cycle. Now, she wonders if that’s even feasible.
“It’s really emotional to have only one embryo left,” Caron said. “I feel like I can’t wait until next year, until after the elections.”
She and her husband had considered moving their embryo to another state, but they were scared off by stories of IVF cycles “not going well” after an embryo has been moved, though typically the process is safe. Then there’s the financial component: To move her embryo to another state and then travel for a subsequent transfer would mean thousands more dollars over the $40,000 they’ve already spent.
“I know I want to try to have another child. I know I want to transfer this embryo. But I want to do it on my terms, when I am ready,” Caron said.
But if she lost the baby because the state rushed her into a decision, “I will blame myself forever,” she said.
The situation is not too far removed from the one abortion patients face — losing choice means losing the autonomy to dictate their own future. Those decisions would instead be for someone else to decide, and for them to absorb.
“I am so upset that my choice and my timeline to expand my family was taken away from me when any other person who can have a child naturally can choose when they want to have that baby,” Caron said. “It’s already so stressful as is, and now to not feel in control — I feel like I just have to jump off the diving board.”