What do you want to know about health care? We want to hear from you, our readers, about what we should be reporting and how we can serve you. Get in touch here.
Most health insurance plans must for now continue to cover preventive services, including the HIV prevention pill, with no out-of-pocket costs for consumers, under a deal reached between the Department of Justice and a group of employers in Texas.
The agreement is in effect while this case, which challenges the Affordable Care Act’s requirement that insurance plans cover certain preventive medical care without requiring any out-of-pocket payments from patients, is litigated in front of the U.S. Court of Appeals for the 5th Circuit. The Texas-based employers have contested the authority of several government task forces — called U.S. Preventive Services Task Force, the Health Resources and Services Administration, and the Advisory Council on Immunization Practices — to determine which preventive services must be covered.
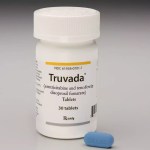
The deal, which was approved by the appeals court, ensures that at least for now, the HIV prevention medication known as pre-exposure prophylaxis, or PrEP, will remain affordable and accessible.
-
Previous Coverage:
The agreement also affects a range of other reproductive health services that insurance plans currently must cover with no copays, including HIV screening, chlamydia and gonorrhea screenings, breastfeeding support, mental health interventions for pregnant and postpartum people, and counseling and treatment for people at higher risk of breast cancer.
The employers who filed suit over the requirements have argued that they should not have to buy insurance that covers contraception, claiming that doing so violates their religious freedom. Currently, the ACA requires that health insurance plans cover at least one version of each form of birth control, without requiring people pay anything out of pocket.
They have made the same argument about buying insurance that covers PreP, claiming that both benefits make them “complicit in facilitating homosexual behavior, drug use, and sexual activity outside of marriage between one man and one woman.” But so far, courts have not been friendly to those arguments.
-
Read Next:
This agreement is hardly the last word. The deal determines only what benefits health insurance plans must provide while this case is being litigated.
The judges will soon weigh in on the merits of the case itself — whether the ACA’s preventive services requirement is constitutional at all — and could still decide to undo that mandate entirely. Doing so could open up consumers, particularly women and LGBTQ+ people, who are more likely to use these benefits, to health costs that they have not had to pay for years, gutting one of the health law’s most significant gender-based benefits. Depending on how the 5th Circuit rules, this case could ultimately end up before the Supreme Court.