At this point in the pandemic, there are a few knowns. One of the biggest ones? That pregnant people are more likely to have severe cases of COVID-19 compared to non-pregnant people.
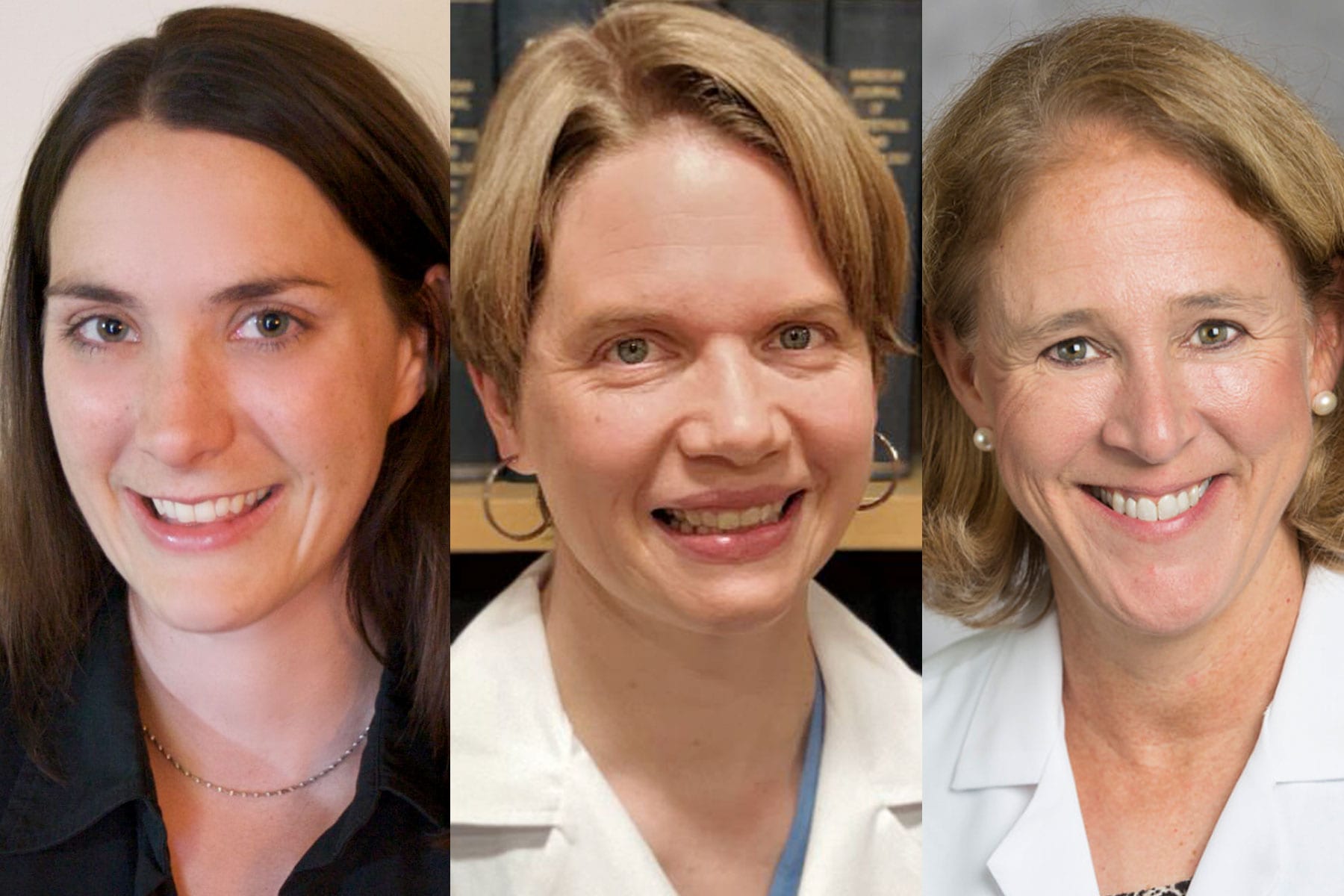
“The number one reason to counsel pregnant patients to take safety precautions and encourage vaccination is because we know pregnant individuals get sicker,” Dr. Kathryn J. Gray, the attending physician in the department of maternal-fetal medicine at Brigham and Women’s Hospital and an assistant professor at Harvard Medical School told The 19th.
Historically, pregnant people have been excluded from medical and pharmaceutical clinical trials out of ethical concerns and this was also true in all of the COVID vaccine trials. It’s a move, though, that is out of step with the guidance of major medical organizations who are pushing back on this stigma and default unofficial policy. Gray said pregnant people were put in a “terrible spot” by being left out of the clinical trials for COVID vaccines that were then granted Emergency Use Authorization by the Food and Drug Administration (FDA).
That is part of the reason she and some of her colleagues at Brigham and Women’s and Massachusetts General Hospital began to research what the antibody response to vaccines was in pregnant people and whether any of these protective antibodies were passed along through the placenta or, after birth, through breast milk.
The answer? Yes. But also? Not in the same way a vaccine protects an adult.
“Pregnant people have similar antibody levels following COVID vaccination as non-pregnant people,” Gray said of what she learned about the COVID vaccine from her own research. “And all pregnant individuals with vaccine-induced antibodies passed these antibodies through the placenta to their babies’ cord blood and to breast milk. So it’s likely that there is some benefit to baby from maternal vaccination.”
The protective antibodies that have been found in cord blood reach a newborn baby through the placenta, and they produce what’s known as passive immunity, said Gray. Passive immunity means that these babies “have some antibodies from mom, and we think that this provides them with some level of protection.” Some comes, Gray said, because these transplacentally conferred antibodies are thought to stick around in a baby’s immune system for somewhere from a few weeks to six months.
But by six months of age, Gray explained, those antibodies would be likely gone because a baby’s immune system wouldn’t be able to produce them on their own. This is why Gray said that when a COVID vaccine is available for young children, likely in September for children ages 2 through 12, and could be available for infants as young as six months, vaccination remains the best way to confer protection.
With breastfeeding, the potential for immunity is less significant as the maternal antibodies are consumed by a baby through breastmilk and then go into the gut, and not directly into the baby’s own bloodstream. “We know that breastfed infants are less likely to have some kinds of infection when they are infants, but whether that will turn out to be true from the antibodies from the COVID vaccine remains to be seen,” Gray said.
But what about parents who were infected with COVID-19 during pregnancy? Wouldn’t they pass on antibodies as well?
The research on that was less clear.
Dr. Carolynn Dude, an assistant professor of maternal fetal medicine at Emory University, helped lead a study on that subject. The results, which appear in the most recent issue of the journal Obstetrics and Gynecology, show that while parents were found to have mounted a robust immunological response after contracting COVID, with a significant of neutralizing antibodies present in their blood samples at the time of delivery, these same protective antibodies were found in only 25 percent of infants born to these same patients.
This, Dude said, suggested that the vaccines might offer more protection to babies than a parent’s bout with the disease.
How do doctors balance questions about vaccines of any kind, and especially the COVID vaccine? “We don’t want to expose a potential harm without a potential benefit,” Dude told The 19th. But, she added, “the vaccination benefits are real.” Dude also clarified that these benefits apply to not only pregnant women, but all pregnant people.
Yet another paper in the new issue of Obstetrics and Gynecology continues to round out the evidence that not only is the COVID vaccine safe for pregnant people, but confers immunity to a fetus that they otherwise couldn’t get, whether through natural infection in their parent or being too young to be vaccinated in their own right once born. Researchers from Weill-Cornell Medical Center found protective antibodies present in the cord blood of 99 percent of those babies born to a parent who had been vaccinated while pregnant with them.
“We know a lot about maternal vaccination,” said Dr. Denise Jamieson, chair of the Department of Obstetrics and Gynecology at Emory University’s School of Medicine and a spokesperson for the American College of Obstetricians and Gynecologists, pointing specifically at the decades worth of data on influenza and TDAP vaccines on pregnant people. “We know that by getting vaccinated for the flu during pregnancy, this protects not only yourself, but protects the baby. That’s important because the baby is too young to get vaccinated at birth, and this provides critical protection in a window for a baby until they are old enough to get vaccinated.” Similarly, Jamieson explained, the TDAP vaccine is routinely given during pregnancy not for the health of the pregnant person, but with the intent of protecting the fetus after birth. So far, signs point to COVID vaccination having the same transplacental effect.
Many of those included in Dude’s research presented with completely asymptomatic COVID cases, and self-reported being careful with COVID precautions such as masks, social distancing, and hand washing. This finding was a key representation of what is so difficult about COVID — and so potentially risky for pregnant people. “Risk assessment is hard in this pandemic, especially around your individual choices,” Dude said. “But we have no solid data to say that vaccines are harmful, and lots of data that COVID is harmful to pregnant people.”
Jamieson noted that this latest round of research — including a third paper in this month’s Obstetrics and Gynecology that found that COVID vaccination does not cause placental damage in the way that organic infection potentially can — demonstrates that more likely than not, these vaccines are not only safe in pregnant populations, but critical for positive health outcomes for the pregnant person and baby both.
“It’s so hard to measure how much protection a baby will have from a vaccinated mother,” said Gray. “Which is why I return to the importance of adults getting vaccinated. If all caregivers are vaccinated, this concept of cocooning means they are much less likely to bring home the infection. All adults should receive vaccination. That’s the best system for protecting infants that we have right now.”